
AI that perfectly matches staffing with demand.
Whether you're planning next month’s schedule or next year’s hiring needs, stay ahead of the curve with Workforce AI technology.
Book a demo
Forecast when — and where — resources are needed most
Workforce AI uses predictive analytics, AI and machine learning to forecast patient demand and workforce needs months in advance, ensuring you always have the right resources in place at the right time.
With three distinct modules for hiring, scheduling and staffing, Workforce AI provides actionable recommendations that optimize labor costs, improve resource allocation and free up your time to focus on other important tasks.
Maximize FTE utilization
Easily integrates with HRIS, VMS and scheduling tools
Spend less on premium labor
Save hours per week of manual effort
Achieve complete harmony between hiring, scheduling and staffing – powered by AI
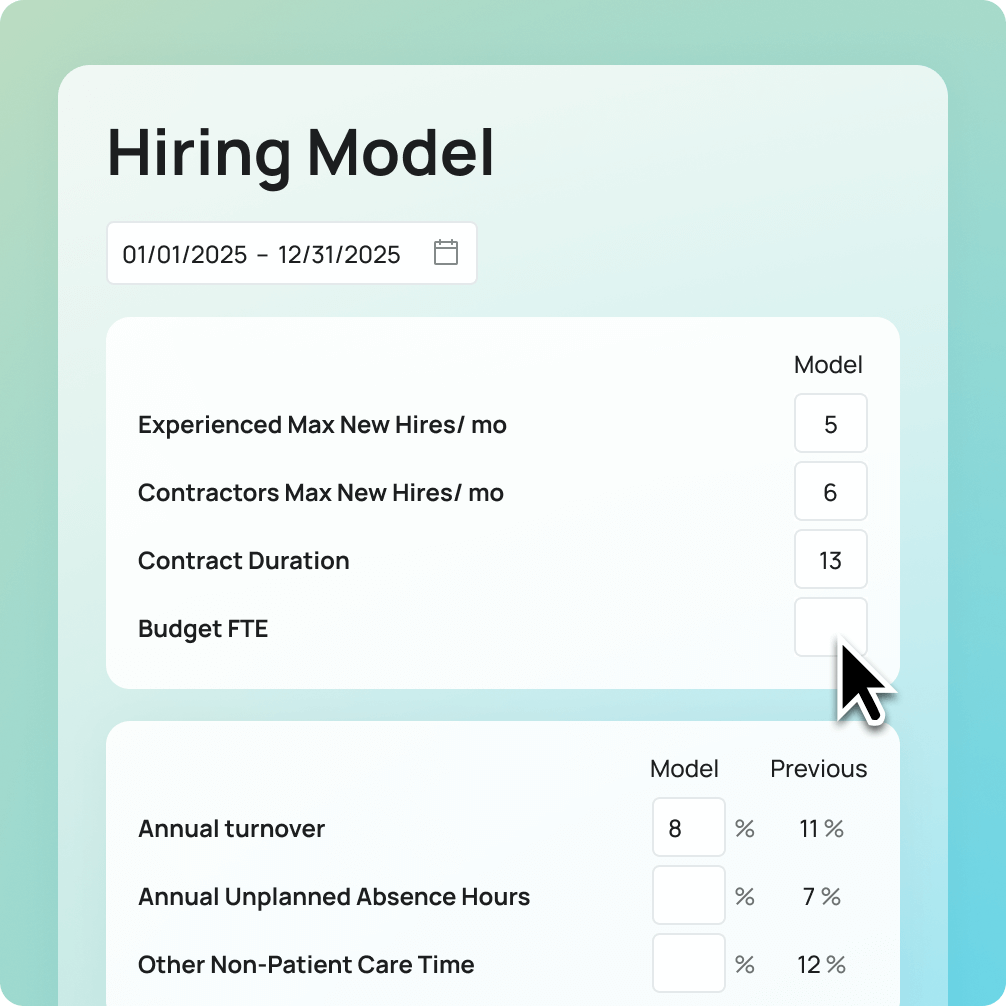
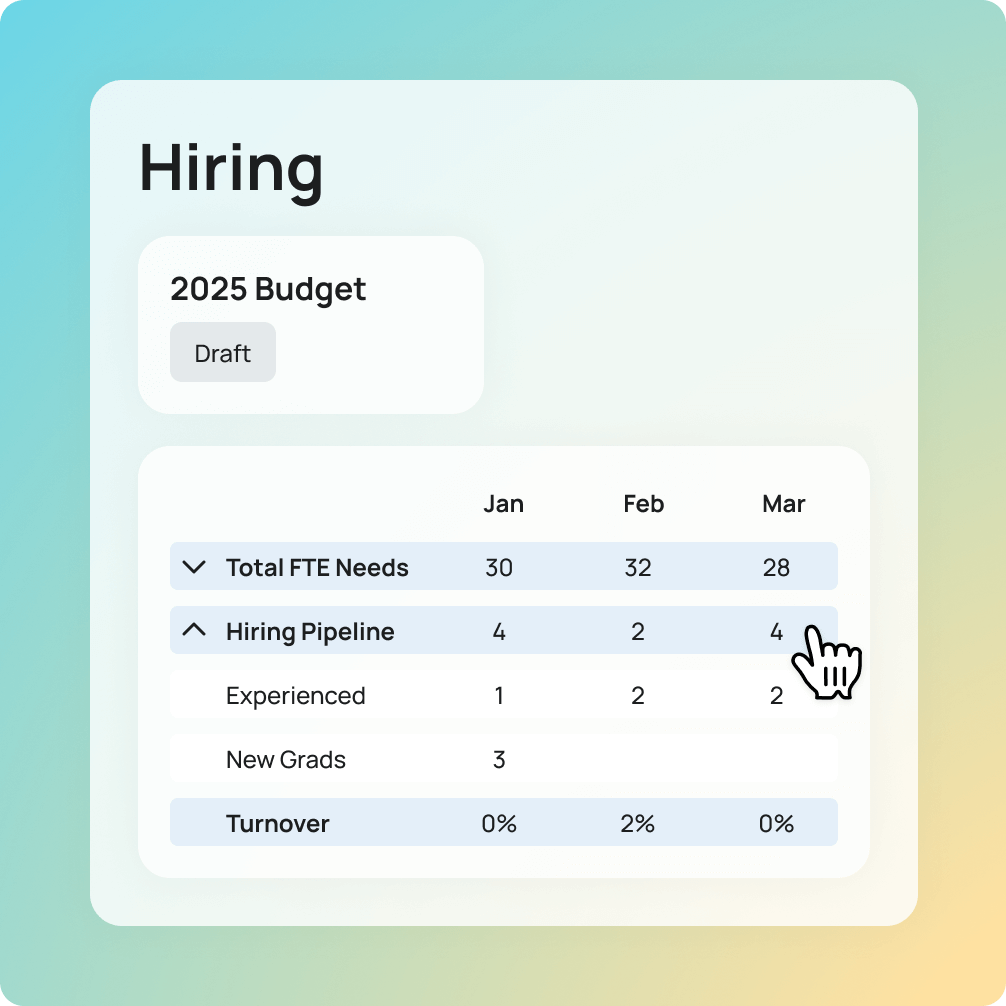
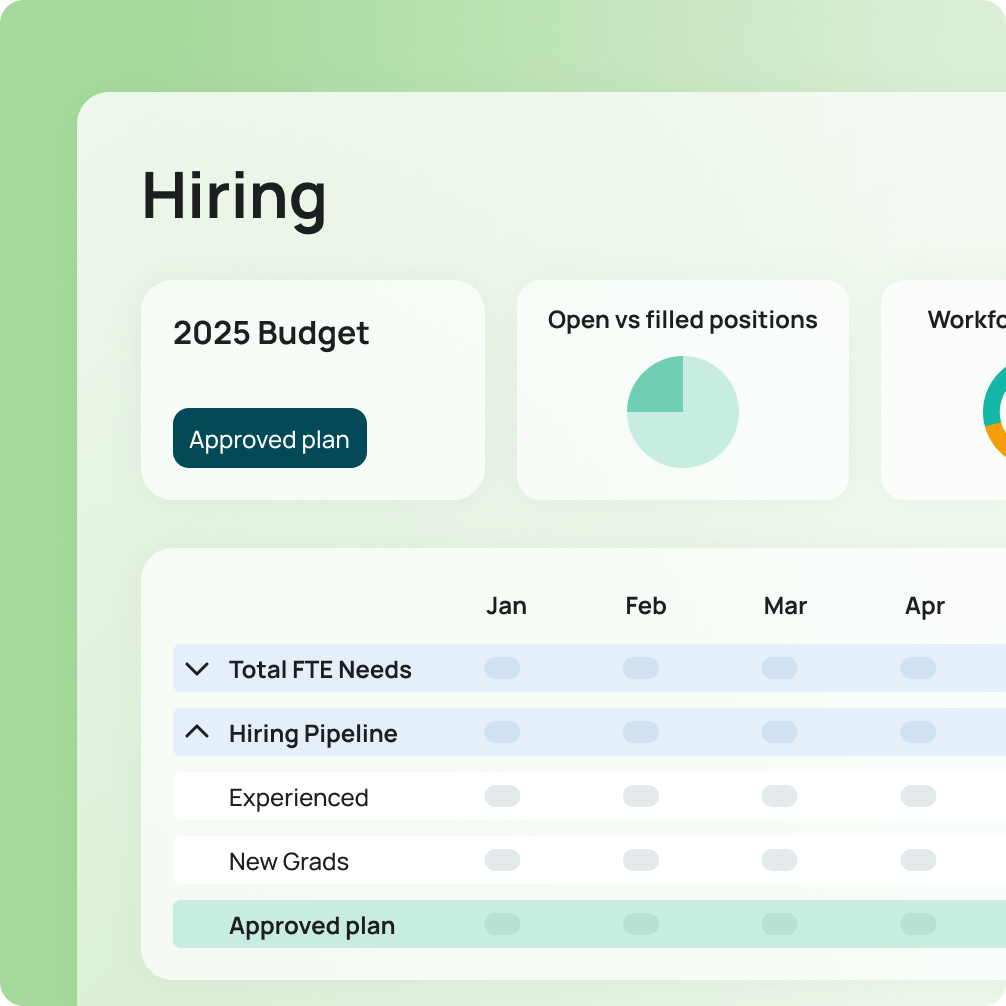
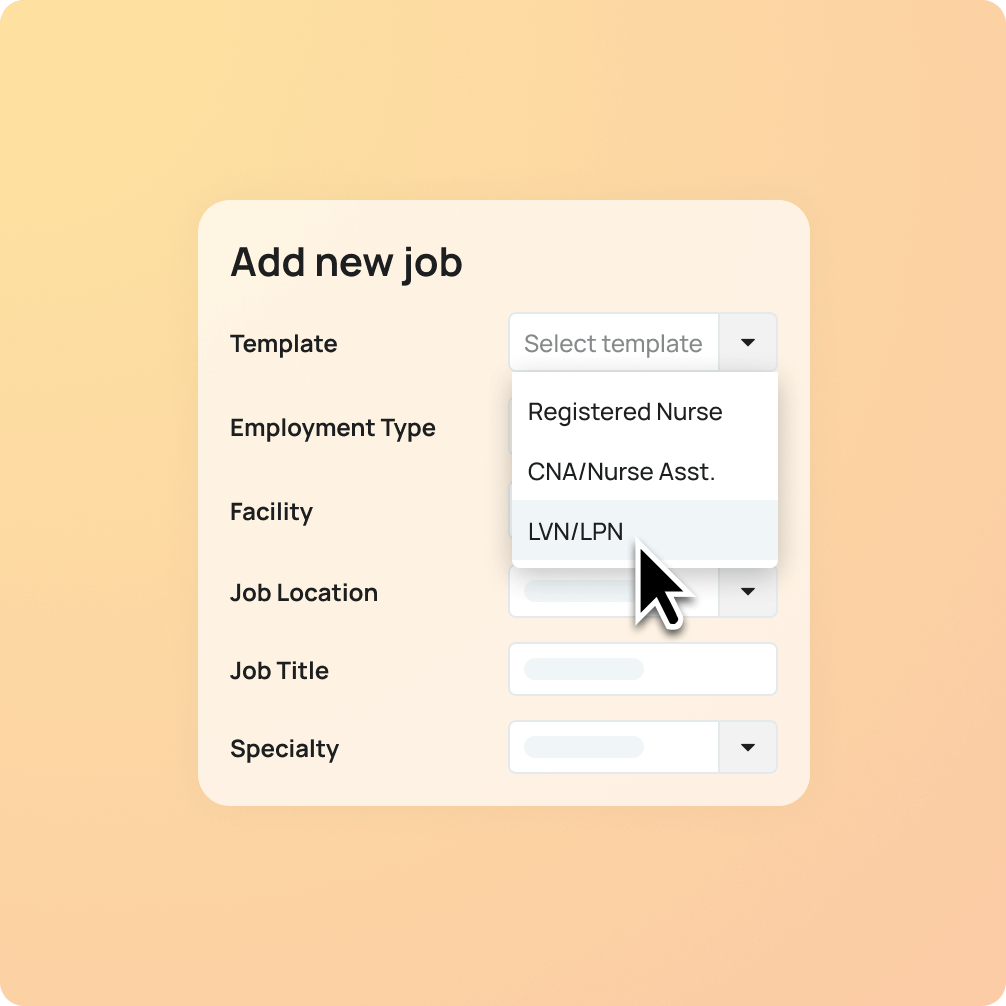
Workforce Planning
Take the guesswork out of hiring and anticipate future needs months in advance.
- Model what-if scenarios to prevent under- and over-hiring
- Get guidance on budgeting for core and contingent labor
- Anticipate hiring needs 12 months in advance
- Easily push job requisitions to LotusOne to fill open roles quickly
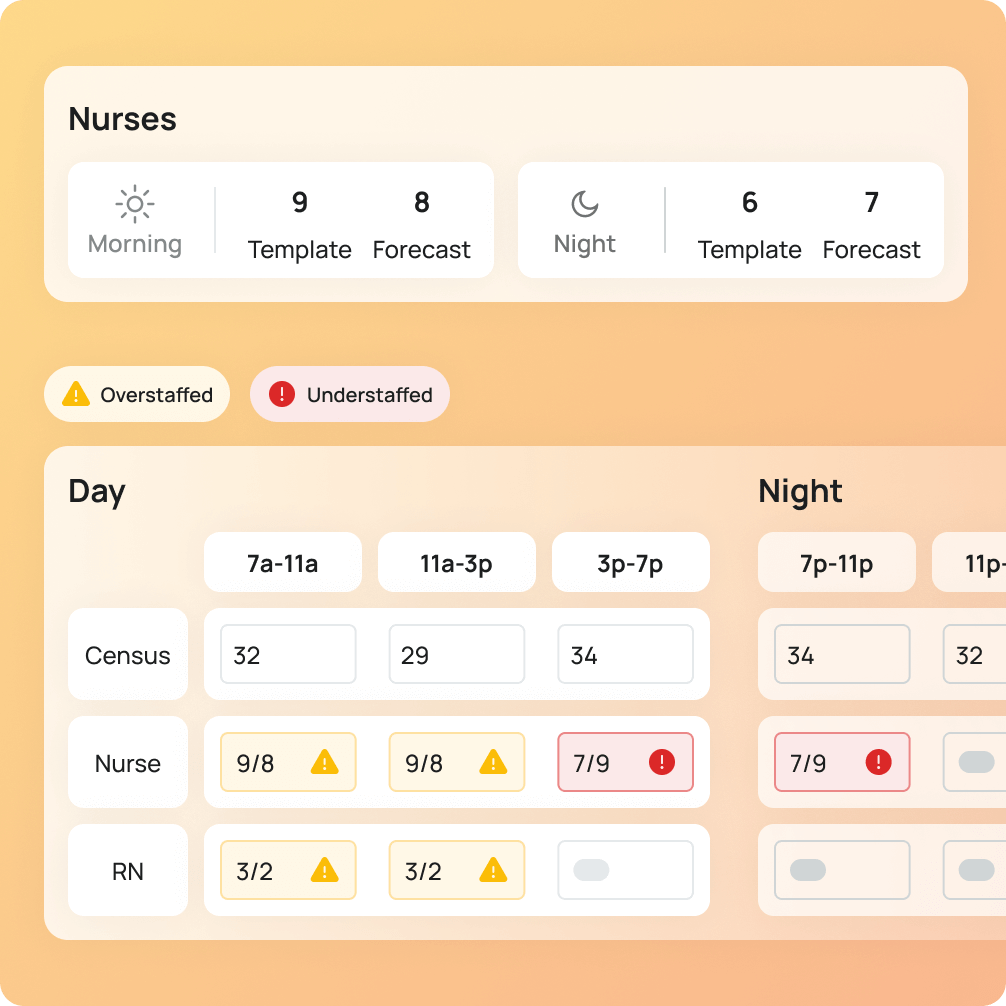
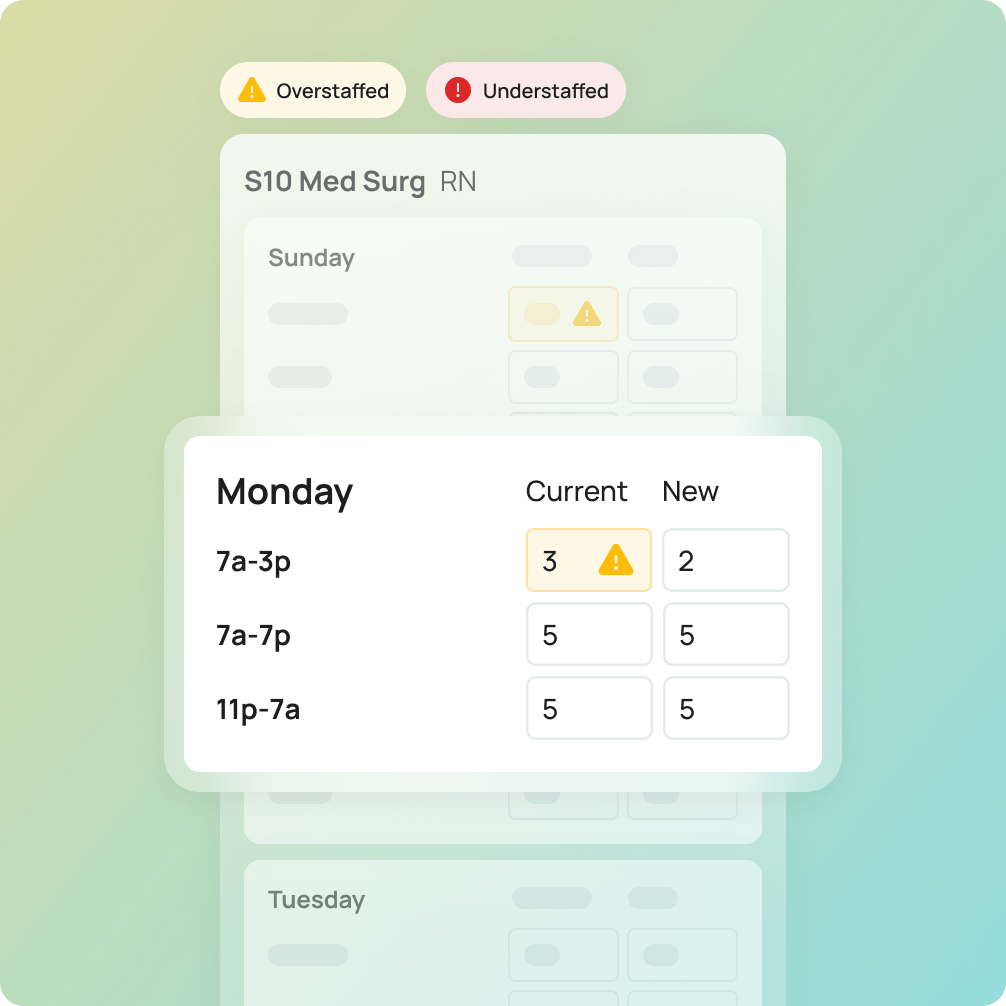
Predictive Scheduling
Automatically create and balance schedules for improved staffing accuracy.
- Create schedule templates aligned with forecasted demand
- Resolve staffing issues for upcoming schedule cycle
- Auto-balance schedules with AI
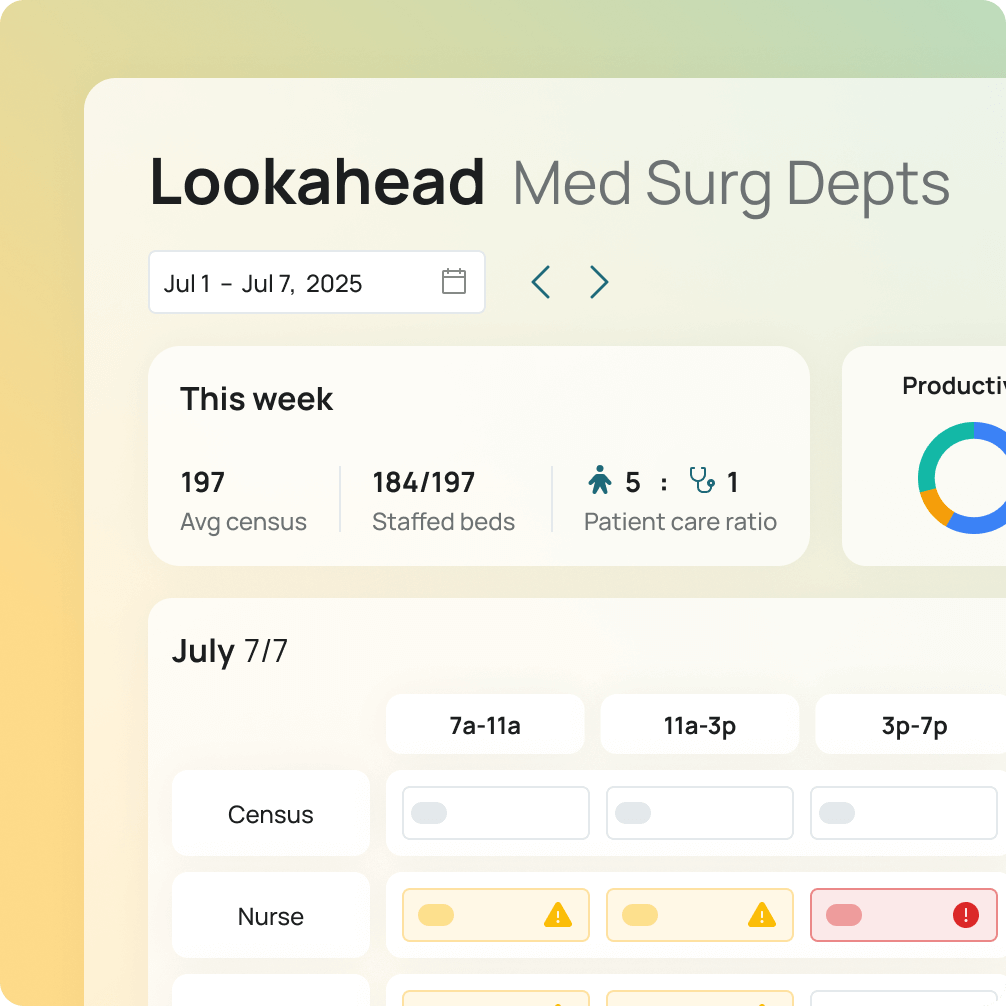
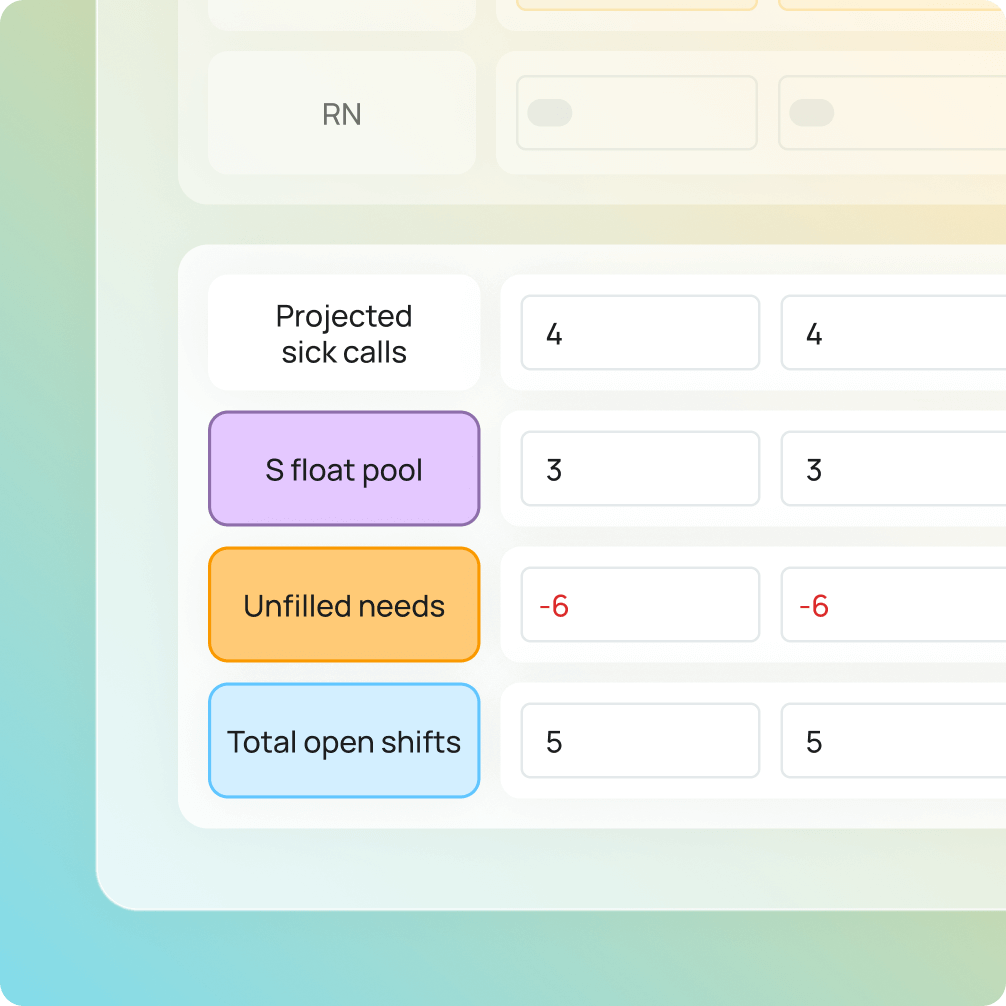

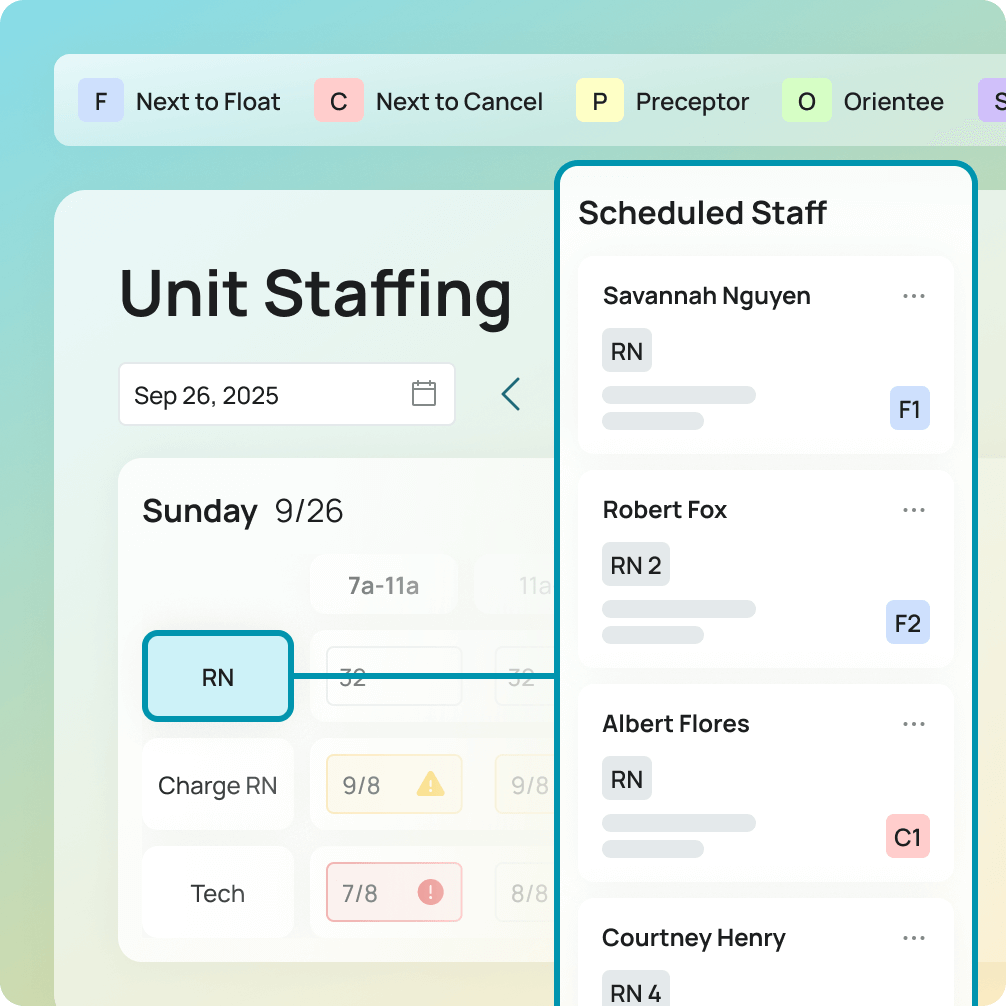
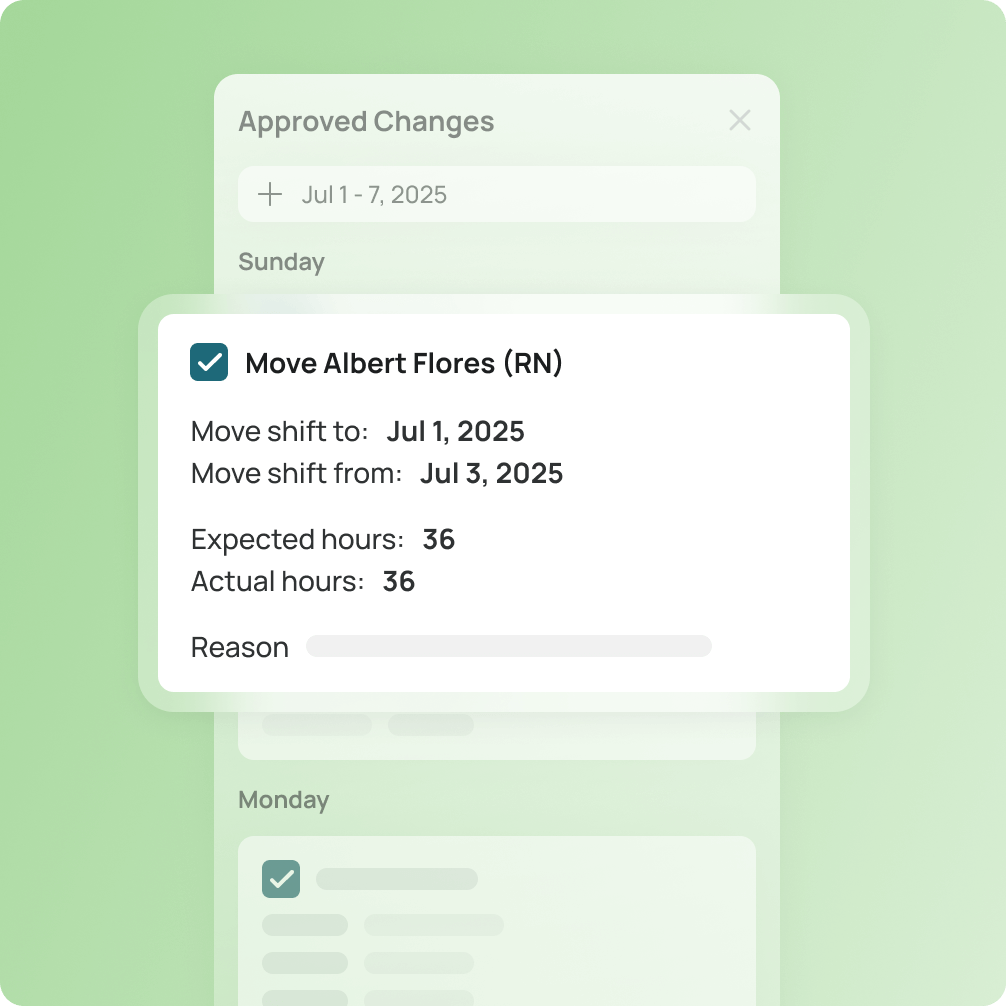
Predictive Staffing
Manage active schedules to meet real-time staffing demands.
- Manage active schedules and view open shifts across multiple departments or clusters
- Forecast call-offs and no-shows to address critical staffing needs weeks in advance
- View trends for open beds, volume and ADT by department
- Automate staffing plan creation with recommendations for next to float, cancel or place on standby
Data‒driven workforce insights
Get more out of your data
Workforce AI technology integrates seamlessly with your HRIS, VMS and scheduling tools to deliver actionable insights from your data.

Our Workforce AI technology makes workforce management simple.
Request a demo today to learn more.
